Clinical information
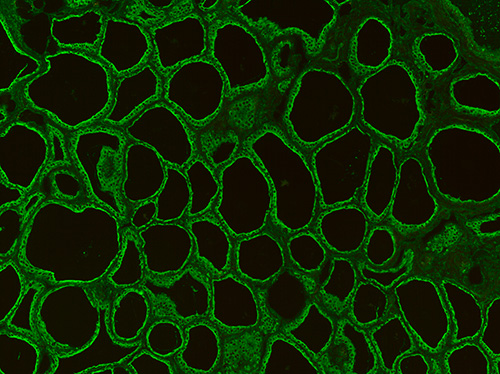
Autoimmune thyroid diseases are the most common type of autoimmune diseases. In the blood of the patients, autoantibodies can be detected which are directed against different thyroid proteins and impair their functioning. Antibodies against thyroid microsomes, with their main antigen thyroperoxidase (anti-TPO), and antibodies against thyroglobulin (anti-TG) or the thyroid-stimulating hormone receptor (TRAb) are characteristic of autoimmune thyroid diseases. The most frequent autoimmune thyroid diseases are Graves’ disease and Hashimoto’s thyroiditis. While Graves’ disease is associated with hyperthyroidism, Hashimoto’s thyroiditis manifests as hypothyroidism.
Graves’ disease is the most frequent cause of hyperthyroidism in individuals with a sufficient iodide supply. It usually has a sudden onset, with initial symptoms such as palpitations and nervousness. The prevalence of Graves’ disease is approximately 1.5%. The number of affected women is eight times higher than that of men. Graves’ disease is characterised by the continuous stimulation of TSH receptors through the binding of TRAb. They act as TSHR agonists and lead to increased iodide uptake, resulting in thyroid growth and increased thyroid-hormone synthesis and release. Main symptoms are struma, tachycardia and endocrine orbitopathy.
The prevalence of Hashimoto’s thyroiditis is 2% in women and 0.2% in men. In contrast to Graves’ disease, the onset of Hashimoto’s disease is usually clinically inconspicuous and can lead to hypothyroidism after years. The majority of cases develop struma. Typical symptoms are cold intolerance, constipation and fatigue. The underlying cause of the disease is autoimmune lymphocytic infiltration, which leads to T-cell-mediated destruction of the thyroid tissue and thus to reduced production of the thyroid hormones triiodothyronine (T3) and thyroxine (T4) in the long term. The antibodies characteristic of Hashimoto’s thyroiditis are anti-TPO and anti-TG.
Postpartum thyroiditis (PPT) is a de novo autoimmune disease that occurs in approximately 5% to 9% of women within one year of delivery and is associated with high titers of anti-TPO and/or anti-TG. The risk of developing the disease is particularly high if the mothers already exhibited thyroid antibodies or had been diagnosed with diabetes mellitus 1 beforehand. The majority of affected women have transient hypothyroidism. But a hyperthyroid phase followed by a hypothyroid phase or isolated thyrotoxicosis can also occur. In 20% to 40%, hypothyroidism persists beyond the postpartum period.
Diagnostics
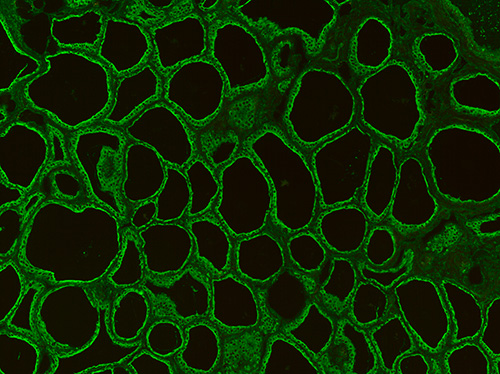
If thyroid disease is suspected, a thyroid function test should be performed to supplement the clinical picture. A thyroid function test is used to determine the TSH concentration in the blood. An increased TSH level indicates hypothyroidism and a decreased level hyperthyroidism. Additionally, the levels of the free thyroid hormones fT3 and fT4 should be measured in the blood. For the differentiation of an autoimmune thyroid disease from acute (bacterial) or subacute (non-infectious) thyroiditis or a non-autoimmune disorder of the thyroid hormone regulation, the determination of antibodies against thyroid antigens is useful. TRAb are the most important serological markers of Graves' disease, as these antibodies can be detected in almost all untreated patients. The TRAb concentration correlates with the disease activity. In a mild course, it may be in the normal range. In these cases, the detection of anti-TPO can support the diagnosis, as these antibodies are found in 90% and anti-TG in up to 30% of Graves’ disease cases. In Hashimoto’s thyroiditis, anti-TPO are found in about 95% of patients, anti-TG in 60% to 80% and TRAb in 6% to 12%.
For sufficient differential diagnostics, the overall picture obtained from the investigation of different parameters must be evaluated. In addition to the serological results, the clinical picture and the results of further examinations such as ultrasound examination or scintigraphy must be taken into account.